Search
- Page Path
- HOME > Search
- Clinical Study
- Comparison of the Efficacy and Safety of Insulin Detemir Administered Once Daily According to Two Titration Algorithms (3-0-3 and 2-4-6-8) in Patients with Type 2 Diabetes Mellitus
- Hea Min Yu, Kang Seo Park, Jun Hwa Hong, Keun Yong Park, Jong Min Lee, Bon Jeong Ku, Yeo Joo Kim, Tae Kun Oh
- Endocrinol Metab. 2020;35(1):142-148. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.142
- 4,766 View
- 80 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
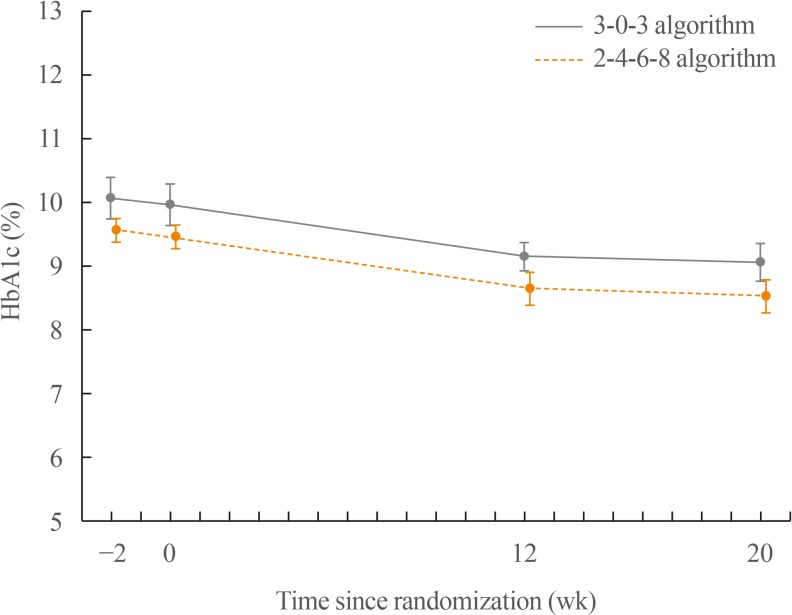
ePub Background This study was conducted to compare glycaemic control with insulin detemir administered according to two titration algorithms (3-0-3 and 2-4-6-8) after 20 weeks of treatment in subjects with type 2 diabetes mellitus inadequately controlled on metformin.
Methods This was a 20-week, randomised, multicentre, open-labelled, treat-to-target trial. Forty-six patients were randomised in a 1:1 manner to either the 3-0-3 (G3,
n =23) or 2-4-6-8 (G2,n =23) algorithm. The primary endpoint was change of haemoglobin A1c (HbA1c), and the secondary safety endpoint included hypoglycaemic events.Results After 20 weeks, HbA1c decreased similarly in the G3 and G2 groups, with a mean change of −0.9% from baseline. The mean change in fasting plasma glucose was numerically similar in both groups. The hypoglycaemia event rate per 100-patient-years of exposure (
r ) in the G2 group (r =1,427) was higher than that in the G3 group (r =807).Conclusion Both treatment groups had numerically similar HbA1c reductions. A trend towards fewer hypoglycaemia episodes after dose stabilisation was seen with the simpler G3. Clinically, this may be an important observation, as a simpler titration algorithm may support self-management and maintenance of insulin therapy.
-
Citations
Citations to this article as recorded by- Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance
Camilla Heisel Nyholm Thomsen, Stine Hangaard, Thomas Kronborg, Peter Vestergaard, Ole Hejlesen, Morten Hasselstrøm Jensen
Journal of Diabetes Science and Technology.2022; : 193229682211459. CrossRef - Efficacy and safety of patient-led versus physician-led titration of basal insulin in patients with uncontrolled type 2 diabetes: a meta-analysis of randomized controlled trials
Marco Castellana, Filippo Procino, Rodolfo Sardone, Pierpaolo Trimboli, Gianluigi Giannelli
BMJ Open Diabetes Research & Care.2020; 8(1): e001477. CrossRef
- Time for Using Machine Learning for Dose Guidance in Titration of People With Type 2 Diabetes? A Systematic Review of Basal Insulin Dose Guidance

- A Case of Painless Thyroiditis Followed by Graves' Disease.
- Gyeong Jae Na, Ji Hyun Kim, Se Yoon Park, Ki Won Kim, Hee Ja Ko, Sung Wan Jeon, Yeo Joo Kim, Sang Jin Kim
- Endocrinol Metab. 2012;27(2):147-150. Published online June 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.2.147
- 2,250 View
- 36 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - A 30-year-old man was admitted to our hospital because of fatigue, palpitation and severe weakness of both legs. The admission laboratory findings revealed thyrotoxicosis, and 131I thyroid scintigraphic imaging revealed a low radioactive iodine uptake. He was treated for painless thyroiditis for about 4 months. However, thyrotoxic state had continued and radioactive iodine uptake was markedly increased in the follow up scan. Painless thyroiditis often relapses, but rarely develops into Graves' disease. This is a rare case in which painless thyroiditis was followed by Graves' disease.
-
Citations
Citations to this article as recorded by- A Case of Severe Recurrent Painless Thyroiditis Requiring Thyroidectomy
So Hyun Park, Il Seong Nam-Goong, Young Il Kim, Yun Sun Kim, Yung Min Kim, Eun Sook Kim
Journal of Korean Thyroid Association.2015; 8(1): 113. CrossRef
- A Case of Severe Recurrent Painless Thyroiditis Requiring Thyroidectomy

- Papillary Thyroid Carcinoma Manifesting as an Autonomously Functioning Thyroid Nodule.
- Ji Hyun Kim, Gyeong Jae Na, Ki Won Kim, Hee Ja Ko, Sung Wan Jeon, Yeo Joo Kim, Sang Jin Kim, Hyeun Duk Jo, Chang Jin Kim
- Endocrinol Metab. 2012;27(1):59-62. Published online March 1, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.1.59
- 66,277 View
- 31 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Hyperfunctioning thyroid carcinoma is very rare. Hence, radionuclide imaging of thyroid hot nodules usually suggests a benign tumor, and less than 4% of cases have been reported as malignant. We would like to present a case of a hyperfunctioning papillary thyroid carcinoma that was initially treated with radioactive iodine. A 58-year-old woman was referred to our hospital for palpable thyroid nodule and a 5-kg weight loss within 6 months. Thyroid function test revealed thyrotoxicosis, and thyroid autoantibodies were absent. 99mTc thyroid scintigraphy showed a 2 x 2 cm-sized hyperactive hot nodule at the left lobe. Despite radioactive iodine treatment with a dose of 10 mCi 131I, thyroid function did not improve. Fine needle aspiration revealed papillary thyroid cancer. The patient underwent total thyroidectomy. Although clinical features and thyroid scans suggest a benign nodule, the possibility of malignancy should not be ruled out. Malignant thyroid hot nodules are rare; however, its possibility should be taken into account. Therefore, we suggest that ruling out malignancy by existing diagnostic guidelines can misdiagnose even a typical case with benign features. As thyroid nodule detection is getting sensitive and accurate, we present this case to discuss whether additional diagnostic approaches would be necessary for thyroid nodules.
-
Citations
Citations to this article as recorded by- Ultrasonographic Characteristics of the Hyperfunctioning Thyroid Nodule and Predictive Factors for Thyroid Stimulating Hormone Suppression
Won Sang Yoo, Hoon Sung Choi
International Journal of Thyroidology.2019; 12(1): 35. CrossRef - Papillary Thyroid Carcinoma Presented as a Hot Nodule with Hyperthyroidism
Sung Hye Kong, Seo Young Lee, Ye Seul Yang, Jae Hoon Moon
International Journal of Thyroidology.2016; 9(1): 47. CrossRef
- Ultrasonographic Characteristics of the Hyperfunctioning Thyroid Nodule and Predictive Factors for Thyroid Stimulating Hormone Suppression

- A Case of Primary Hypothyroidism with Anti-Triiodothyronine Autoantibody.
- Jae Ho Park, Ji Hoon Ahn, Mi Hee Kang, Jong Chul Won, Kyung Wook Lee, Yeo Joo Kim, Ji Oh Mok, Hyeong Kyu Park, Chul Hee Kim, Sang Jin Kim, Dong Won Byun, Kyo Il Suh, Myung Hi Yoo
- J Korean Endocr Soc. 2006;21(5):428-432. Published online October 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.5.428
- 1,873 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Antithyroid hormone autoantibodies can be present in the sera of patients with thyroid and non-thyroid disorders. Antithyroid hormone autoantibodies in a patient's serum interfere with radioimmunoassay of thyroid hormones. Clinically, this interference can result in discordance between the serum thyroid hormone levels and the clinical features of the patient, which can lead to misdiagnosis or inappropriate treatment. We experienced a woman who had primary hypothyroidism with unexpectedly high concentrations of serum total triiodothyronine (T(3)) and free T(3), and she had been treated for Graves' disease in the past. Through the use of a polyethylene glycol precipitation method, we detected the anti-triiodothyronine autoantibodies in her serum. We report on this case along with a review of the related literature.
-
Citations
Citations to this article as recorded by- Thyroxine (T4) Autoantibody Interference of Free T4 Concentration Measurement in a Patient With Hashimoto’s Thyroiditis
Mi-Na Lee, Soo-Youn Lee, Kyu Yeon Hur, Hyung-Doo Park
Annals of Laboratory Medicine.2017; 37(2): 169. CrossRef
- Thyroxine (T4) Autoantibody Interference of Free T4 Concentration Measurement in a Patient With Hashimoto’s Thyroiditis

- A Case of Panhypopituitarism with Rhabdomyolysis.
- Sung Wook Hong, Eun Jung Lee, Ji Young Park, Ji Sung Yoon, Ji O Mok, Yeo Joo Kim, Hyeong Kyu Park, Jae Woo Kim, Chul Hee Kim, Sang Jin Kim, Dong Won Byun, Kyo Il Suh, Myung Hi Yoo
- J Korean Endocr Soc. 2005;20(2):174-178. Published online April 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.2.174
- 1,509 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Rhabdomyolysis is the consequence of extensive muscle injury with the release of muscle cell constituents into plasma. It can arise from trauma and also from a variety of nontraumatic causes. Trauma, drugs, toxins and infection are the major causes of rhabdomyolysis, but it is rarely associated with metabolic disorders such as severe electrolyte disturbance, diabetic ketoacidosis, hyperosmolar nonketotic coma, hypothyroidism and thyrotoxicosis. There have been several reported cases of metabolic rhabdomyolysis, but panhypopituitarism as a cause has never been identified. We experienced a case of acute rhabdomyolysis associated with panhypopituitarism. Thus, So we report this case with the review of related literature. Metabolic disorder is a rare cause of rhabdomyolysis, but it should always be considered in a patient having and unexplained increased of the creatine kinase concentration

- A Case of Kallmann's Syndrome with Unilateral Renal Aplasia and Diabetes Mellitus.
- En Jung Lee, Sung Wook Hong, Yun Ki Hong, Ji Sung Yoon, Ji O Mok, Yeo Joo Kim, Hyeong Kyu Park, Chul Hee Kim, Sang Jin Kim, Dong Won Byun, Won Kyung Bae, Kyo Il Suh, Myung Hi Yoo
- J Korean Endocr Soc. 2005;20(1):96-102. Published online February 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.1.96
- 2,079 View
- 41 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Kallmann's syndrome is defined as the combination of hypogonadotropic hypogonadism and anosmia/hyposmia. The syndrome is a result of defect in the embryonic migratory pathway of gonadotropin-releasing hormone, which synthesizes neurons and olfactory axons. The hypogonadotropic hypogonadism results due to absence of or incomplete pubertal development and may be associated with anosmia, hyposmia, midline defect(color blindness, cleft-lip, cleft-palate, unilateral renal agenesis, sensorineural deafness), cryptorchidism and skeletal anomaly. Till date in Korea, few cases of Kallmann's syndrome have been reported but there are no available reports on cases of Kallmann's syndrome with unilateral renal aplasia and diabetes mellitus. We handled a case of Kallmann's syndrome associated with unilateral renal agenesis and diabetes mellitus. In the current work, we present a peculiar case as afore mentioned with the review of related literature.
-
Citations
Citations to this article as recorded by- A Case of Kallmann's Syndrome with Frontal Lobe Atrophy and Mental Retardation
Soyoung Hyun, Seungguk Park, Dong Gu Kang, Seung Uk Jeong, Dea Ho Lee, Gwanpyo Koh
Endocrinology and Metabolism.2010; 25(2): 142. CrossRef - A Case of Kallmann's Syndrome Mildly Presenting as Secondary Amenorrhea
Na Rae Joo, Cheol Young Park, Hong Ju Moon, Jun Goo Kang, Sung Hee Ihm, Moon Gi Choi, Hyung Joon Yoo, Yul Lee, Ki Won Oh, Sung woo Park
Journal of Korean Endocrine Society.2007; 22(2): 130. CrossRef
- A Case of Kallmann's Syndrome with Frontal Lobe Atrophy and Mental Retardation

- A Case of Thyrotoxic Paraplegia.
- Gun Wha Lee, Jin Woo Park, Ji Sung Yoon, Ji O Mok, Yeo Joo Kim, Hyeong Kyu Park, Chul Hee Kim, Sang Jin Kim, Dong Won Byun, Kyo Il Suh, Myung Hi Yoo, Du Shin Jeong
- J Korean Endocr Soc. 2004;19(4):419-425. Published online August 1, 2004
- 1,086 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - Hyperthyroidism may be associated or present with a variety of neuromuscular disorders, including thyrotoxic myopathy, exophthalmic ophthalmoplegia, periodic paralysis and myasthenia gravis. In contrast to muscle, peripheral nerve involvement in hyperthyroidism is exceedingly rare, and has received little attention. Paraplegia-like weakness during severe hyperthyroidism was first described by Charcot in 1889, and called Basedow's paraplegia' by Joffory in 1894. However, there has been no reported case in Korea. A 38-year-old woman was admitted for evaluation of progressive weakness and a gait disturbance. Her endocrinological results were compatible with hyperthyroidism. The polyneuropathy was also confirmed with sequential electrophysiological studies of the nerves and muscles. Drug therapy for hyperthyroidism resulted in resolution of the clinical neurological symptoms and progressive improvement of electrophysiological findings. Hyperthyroidisms are common medical disorders, which are often accompanied by diverse types of neurological and neuromuscular dysfunctions. All of these neurological manifestations are important, as they can serve as important clues to the diagnosis of a thyroid disorder. Furthermore, they are often related to the patient's presenting complaint. Therefore, the physician must be alert to the diverse manifestations of thyroid dysfunction, as they can lead to the diagnosis of potentially serious but treatable disorders. Herein is reported a case of myopathy and neuropathy associated with hyperthyroidism (Basedow's paraplegia), with a review of the literature

- Increased Activity of Insulin-like Growth Factor binding Protein-4 Protease in H-mole Patients.
- Woo Seok Seo, Dong Won Byun, Ji Oh Mok, Ji Sung Yoon, Yeo Joo Kim, Hyung Kyu Park, Chul Hee Kim, Sang Jin Kim, Kyo Il Suh, Myung Hi Yoo, Hae Hyeog Lee, Soo Kyoon Rah
- J Korean Endocr Soc. 2004;19(4):346-357. Published online August 1, 2004
- 1,117 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Hydatidiform mole (H-mole) is characterized by the neoplastic proliferation of trophoblasts. Only 1~10% of patients with partial H-mole will develop a trophoblastic tumor, but 18~29% of those with complete H-mole will develop a persistent trophoblastic tumor. Therefore, the early diagnosis and monitoring after operation of an H-mole disease are very important. Recently, the pregnancy associated plasma protein-A (PAPP-A) was proved to have a similar role as that of IGF binding protein-4 (IGFBP-4) protease, which has shown an increasing function in fetal growth and development by degradation of IGFBP-4 and an increase in IGF in the serum during pregnancy. Our hypothesis is "the H-mole, which shows placental hyperplasia will also have an IGFBP-4 protease activity, which may be used as in the early diagnosis and monitoring of H-mole disease". METHODS: Serum samples from 6 non-pregnant, 18 pregnant (5 in the 1st trimester, 10 in the 2nd, and 3 in the 3rd), 12 postpartum women and 3 H-mole patients(2 with complete H-mole and 1with partial H-mole) were collected and measured for the -HCG, IGF and PAPP-A levels and IGFBP-4 protease activities by a IGF-II ligand blot analysis and electrophoresis method. The IGFBP-4 protease activity of the serum during normal pregnancy was compared with that of H-mole disease. RESULTS: The results from the in vitro protease assays using recombinant IGFBP-4 determined that IGFBP-4 proteolysis was significantly increased during the first (56%) and second trimesters (90%), but reached a plateau by the third trimester (94%). In H-mole disease diagnosed 11 weeks after conception, the IGFBP-4 proteolytic activity was 97%, which was nearly the same as at terminal pregnancy. This activity gradually decreased to 75% at 1 week, 58.7% at 2 and 33% at 3 weeks after the operation. The -HCG was also decreased from 490,400 to 123,822.7, 1,352.3, and 128.5 mIU/mL at 1, 2 and 3 weeks after the operation, respectively. The PAPP-A level also gradually decreased from 34.87 to 25.5, 12.0 and 2.7 g/mL 1, 2 and 3 weeks after the operation, respectively. However, the IGF decreased from 238.3 to 172.9 ng/mL 1 week after the operation, but increased to 251.4 and 295 ng/mL at 2 and 3 weeks after the operation, respectively. CONCLUSION: These results demonstrated that the IGFBP-4 protease activity was significantly increased during pregnancy, and was extremely elevated durimg the early stages of H-mole disease, but gradually decreased after removal of molar tissue. Therefore, measuring the IGFBP-4 protease activity may play an important role in the early diagnosis and monitoring of H-mole disease

- A Case of Severe Thyrotoxicosis Induced by Hydatidiform Mole.
- Jae Hak Lee, Jong Kun Park, Soon Hyo Kwon, Ji Oh Mok, Ji Sung Yoon, Yeo Joo Kim, Hyung Kyu Park, Chul Hee Kim, Sang Jin Kim, Hae Hyeog Lee, Gye Hyun Nam, Gye Hyun Kwan, Eun Suk Ko, Dong Won Byun, Kyo Il Suh, Myung Hi Yoo
- J Korean Endocr Soc. 2003;18(4):420-425. Published online August 1, 2003
- 1,184 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Human chorionic gonadotropin (HCG) is one of the glycoproteins families synthesized by the placenta, and consists of 2 noncovalently joined subunits, namely, alpha and beta. The alpha and beta-subunits have a structural homology with the alpha and beta-subunits of TSH and LH. The thyrotropic action of HCG results from its structural similarity to TSH, so beta-HCG can bind to the TSH receptor in the thyroid gland. A high level of HCG, accompanied by an increased thyroid hormone level, can be observed in gestational trophoblastic diseases (GTD), such as a hydatidiform mole or a choriocarcinoma. However, the clinical symptoms of hyperthyroidism in GTD are rarely observed. A 27-years-old woman, admitted due to an amenorrhea of 11 weeks duration, with thyrotoxic symptoms, such as weight loss, palpitation, sweating, tremor, heat intolerance and anxiety, was evaluated. Her serum free T4 level was 8 times higher than normal, and her serum beta-HCG level was over 1,000,000IU/L. She had a curettage operation, with the pathological findings of a complete hydatidiform mole. These thyrotoxic symptoms developed due to a hydatidiform mole, and were accompanied with a highly increased serum beta-HCG level. After evacuation of the molar tissue, the thyroid hormone and thyrotoxic symptoms normalized. Here, this case is reported, with brief review of the literature.

- A Case of Delayed Puberty due to Hypoplasia of Anterior Pituitary Gland with Pituitary Stalk Agenesis and Ectopic Neurohypophysis.
- Seung Yong Shin, Jin Young Kim, Seung Jae Yoon, Sung Ki Kim, Seong Bin Hong, Yeo Joo Kim, Moon Suk Nam, Mi Rim Kim, Yong Seong Kim
- J Korean Endocr Soc. 1999;14(3):578-586. Published online January 1, 2001
- 1,056 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - Hypopituitarism is not a common cause of delayed puberty, however it should always be considered, especially if there are such signs as severe dwarfism, dollish face, truncal obesity, small hands and feet, and microgenitalia. Either congenital or acquired, hypopituitarism can be resulted from hypothalamic and hypophyseal lesions. The clinical feature can be diverse depending on age of the patients, rate of progression, degree of hormone deficiency and characteristics of the lesion. The recent high interest in delayed puberty and the improved detection of hypothalamic hypophyseal lesions using combined pituitary fuction stimulation test, brain CT and MRJ, has made the differential diagnosis of hypopituitarism possible as the cause of delayed puberty. MRI has shown hypophyeal hypoplasia accompanied by anterior pituitary hypoplasia and ectopic neurohypophysis in some of the patients with hypopituitasm, and although the anatomical abnormality around the hypophysis in these patients is considered the reason for hypopituitarism, the pathogensis of which has not yet to be known. We, here, report a case of delayed puberty by hypopituitarism due to hypoplasia of anterior pituitary gland, pituitary stalk agenesis and ectopic neurohypophysis with brief review of the litereature.

- A Case of Normal Full Term Delivery after Afrenalectomy for Cushing's Syndrome in a Pregnant Patient.
- Sung Sik Yang, Yong Seong Kim, Yong Bum Cho, Young Wan Kim, Seong Bin Hong, Yeo Joo Kim, Mi Rim Kim, Moon Suk Nam, Sei Joong Kim, Suk Hwan Shin, Byoung Ick Lee
- J Korean Endocr Soc. 1999;14(3):562-567. Published online January 1, 2001
- 998 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - We experienced a case of Cushings syndrome due to adrenal adenoma associated with pregnancy 23th week in a 26 year old female patient. On physical findings, hypertension, moon face, hirsutism, abdominal striae and buffalo hump were noticed. Laboratory findings showed increased serum cortisol, increased 24 hours-urinary cortisol, and decreased plasma ACTH. Abdominal MRI demonstrated 4 cm sized in long diameter, well marginated, and ovoid-shape right adrenal mass. Unilateral total adrenalectomy was performed at the 23th week of pregnancy and the mass it was confirmed to benign adrenal adenoma. Steroid replacement therapy was continued with 7.5 mg prednisolone during remaining pregnancy. At the 38th week of pregnancy, labor was developed and she delivered healthy female weighing 2.5 kg through normal vaginal delivery without complication. Pregnancy rarely occurs in patients with Cushings syndrome. We think she was the first case in Korea who had normal 38th week transvaginal delivery after adrenalectomy in adrenal Cushings syndrome during pregnancy.

- A Case of Aldosteronoma Complicated with Hyperthyroidism.
- Yeo Joo Kim, Mi Rim Kim, Moon Seok Nam, Hyo Young Min, Sung Ryol Kwon, Sung Wook Cho, Young Ub Cho, Yong Sung Kim
- J Korean Endocr Soc. 1998;13(3):480-488. Published online January 1, 2001
- 1,095 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Primary aldosteronism is characterized by hypokalemic metabolic alkalosis, low plasma renin activity, elevated plasma aldosterone level and can be suspected in the patients with hypertension and unexplained hypokalemia. Small adrenal cortical adenomas are responsible for this syndrome in most cases. The incidence of thyrotoxic periodic paralysis ranges from 1.9 to 6.2 % in Japan. Thyrotoxic periodic paralysis usually subsides following treatment of hyperthyroidism and has good prognosis. A 56 year-old man presented with hyperthyroidism, hypertension and recurrent hypokalemia. During the treatment of hyperthyroidism, he repeatedly experienced weakness of both lower extremities. Hormonal evaluation was performed and he was found to have a 2*2*1.5 cm sized right adrenal tumor by abdominal computerized topography(CT). After right adrenalectomy, hypokalemic periodic paralysis was improved. Both thyroid and adrenal function should be comprehensively investigated in periodic paralysis. In conclusion, physicians must be aware of the possibility of primary aldosteronism in hyperthyroid patients with hypokalemic periodic paralysis. We report a case of aldosteronoma complicated with hyperthyroidism and literatures are reviewed.

- A Case of Hyponatremin Encephalopathy Developed after Transsphenoidal Pituitary Sergery in Menstruant Woman.
- Yeo Joo Kim, Mi Rim Kim, Moon Seok Nam, Yong Sung Kim, Jung Bae Jin, Sang Hyun Park, Jun Hong Kang, Sung Bin Hong, Byoung Yun Jun
- J Korean Endocr Soc. 1998;13(3):439-445. Published online January 1, 2001
- 971 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - A 41-year-old female complaining of easy fatigue, headache, thickened extremities and deepened facial folds was admitted to the hospital. As early as 6 years ago, she had been told by family members that her voice was changed and both hands was thickened. Cranial plain radiography indicated ballooning of sella turcica. Sella MRI disclosed 2.2cm sized pituitary tumor with suprasellar extension. The pituitary tumor with hypothalamic extension was removed via a transsphenoidal approach. The postoperative course was uneventful until hyponatremia with sudden headache and respiratory arrest was developed. The case was due to hyponatremic encephalopathy on the basis of the clinical course and symptoms, and 3% hypertonic saline was infused for 12 hours until the hyponatremia was corrected. We have experienced a mortality case of hyponatremic encephalopathy in which surgieal removal of a pituitary tumor from a female acromegalic patient in menstruant period was followed by the sudden occurrence of hyponatremia, which in turn was later associated with marked brain edema.

- Effect of ICV Corticosterone on hypothalamic NPY mRNA Expression in food-restricted, Adrenalectomized Rats.
- Yeo Joo Kim, Mi Rim Kim, Moon Seok Nam, Yong Sung Kim
- J Korean Endocr Soc. 1998;13(2):150-155. Published online January 1, 2001
- 978 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Adrenalectomy does impair the expression of hypothalamic NPY gene in the rat and replacement of glucocorticoid by intracerebroventricular(ICV) route resulted in a normalization of refeeding hyperphagia and weight gain in adrenalectomized(ADX), food-deprived rats. The purpose of this study was to assess the direct effect of CNS glucocorticoid on hypothalamic NPY gene expression which occurs following food deprivation in ADX rats. METHODS: Adult male Wistar rats were fitted with ICV cannulae and restricted the food intake for 14 days. Adrenalectomy and sham operation were done on the 10th day and single ICV corticosterone acetate(100ug/2uL) was given in one ADX group(ADX+CORT, n=9) and vehicle (2uL) was given in another ADX group(ADX+VEH, n=9) and sham rats(SHAM+VEH, n=7). After experiment, we measured NPY mRNA on arcuate nucleus by in situ hybridization. RESULTS: The rate of weight loss of ADX rats closely parallded that of sham-operated rats. Plasma glucose and insulin levels were not significantly different in three groups. Hybridization density on the ARC in ADX+VEH rats(0.42+/-0.02uCi/g: p<0.05) was significantly reduced compared to that in sham controls(0.68+/-0. 11uCi/g). ICV corticosterone injection increased the hybridization density in ADX+CORT rats(0.53+/-0.04uCi/g) compared to vehicle alone, although this did not reach that of controls. NPY gene expression was 40% in ADX+VEH rats and 62% in ADX+CORT rats compared to control rats. CONCLUSIONS: These results are consistent with the hypothesis that CNS glucocorticoid deficiency appears to be responsible for the impairment of refeeding hyperphagia in ADX rats and the effect of CNS glucocorticoid deficiency is a manifestation of impaired activation of hypothalamic NPY gene expression in the ARC.

- A Case of Partial Hypopituitarism after Recovery from Korean Hemorrhagic Fever.
- Yeo Joo Kim, Mi Rim Kim, Moon Seok Nam, Yong Sung Kim, Sung Ki Kim, Sung Kwon Bae
- J Korean Endocr Soc. 1997;12(4):584-588. Published online January 1, 2001
- 989 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Heorrhage and infarct-like necrosis of anterior lobe of the pituitary gland is one of the characteristic pathologic findings of the autopsied cases of Korean Hemorrhagic Fever (KHF) patients, but there has been rare reports of hypopituitarism in patients with KHF. Recently we have experienced a patient with hyponatremia who had recovered from KHF. He was admitted to our hospital due to nausea, vomiting, and epigastric discornfort. To determine the function of the anterior pituitary gland, hormonal levels of target galnds and pituitary gland were measured, and combined pituitary stimulation test was performed. ACTH, GH, and prolactin deficiency were confirmed by combined pituitary stimulation test in this patient. There was no evidence of hypothalamic or other pituitary diseases by brain MRI. Our experience shows that KHF can be a cause of hypopituitarism and these findings should alert physicians the possibility of hypopituitarisrn in patients who had recovered from KHF.


 KES
KES

 First
First Prev
Prev



